
Data on the relationship between long-chain omega-3 PUFAs (n-3 LC-PUFAs) and the risk of developing atrial fibrillation are notoriously inconsistent. Whether examining the risk of incident atrial fibrillation in individuals with no history of the condition, risk following coronary surgery or the odds of recurrent atrial fibrillation, reports vary from reduced risk to no association or, in a rare instance, an
adverse association. Finding ways to lower the risk of atrial fibrillation is important because the condition is associated with an
increased risk of stroke, myocardial infarction ventricular arrhythmia and mortality (Figure). Current risk reduction strategies focus on restoring normal sinus rhythm, controlling symptoms and preventing strokes. There would be considerable patient benefit if one could reduce the risk of developing the condition or reduce or prevent subsequent episodes.
Mixed findings have been reported for the consumption or status of n-3 LC-PUFAs and the risk of incident atrial fibrillation. In a recent study among older US adults without atrial fibrillation, those with higher total n-3 LC-PUFA or DHA levels in blood had a significant 29%
lower risk of the condition compared with those having lower levels. Similar results were reported in a
Finnish study among men. Another study of older US adults observed that those who consumed tuna or other broiled or baked fish 1 to 4 times/week had a significant
28% lower risk of incident atrial fibrillation. A study among patients hospitalized for myocardial infarction reported a
significant reduction in 1-year atrial fibrillation in patients with n-3 LC-PUFA supplementation. In contrast, the
Rotterdam Study of 67-year-old adults without atrial fibrillation observed no association between fish or EPA and DHA consumption with subsequent risk of the condition. Similarly, data from the Women’s Health Initiative indicated
no association between fish or n-3 intakes and risk of the condition among older women. A large cohort study among Danes found
no association between fish consumption and incident atrial fibrillation. In the
Framingham Study, fish consumption was not associated with risk, except in a small number of participants (5 of 21 at risk) who ate more than 4 servings of dark fish per week. These individuals experienced a significantly higher risk of the condition.
Two meta-analyses of randomized controlled trials on the prevention of atrial fibrillation with n-3 LC-PUFAs concluded that these fatty acids were
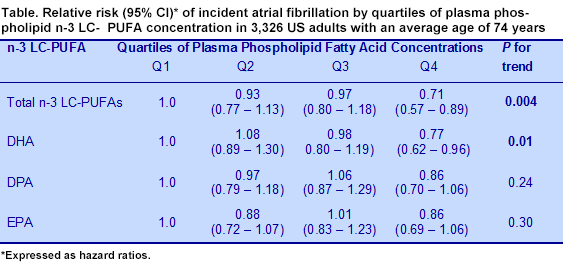
not associated with a reduced risk of developing the condition. Two new studies have reported findings about the consumption of fish or blood levels of n-3 LC-PUFAs and the risk of incident atrial fibrillation in older adults. Jason Wu and colleagues analyzed plasma phospholipid fatty acid data from 3,326 men and women, 74 years of age on average, who were free of atrial fibrillation or heart failure at baseline. Participants were enrolled in the Cardiovascular Health Study, a community-based sample of older adults. The investigators had
previously reported a significant reduction in incident atrial fibrillation among those participants who consumed tuna or other baked fish 1 to 4 times/week. However, analysis of biomarkers avoids the errors associated with dietary intake data.

The investigators measured plasma phospholipid fatty acids approximately 3 years after baseline. In a subset of samples, they evaluated the change in dietary exposure over time using blood samples obtained 13 years after baseline. With these data, they were able to adjust the regression data for regression dilution bias and estimate how usual n-3 LC-PUFA levels relate to atrial fibrillation. Consistent with their previous dietary associations, the investigators observed a significant reduction in the relative risk of incident atrial fibrillation with higher concentrations of total n-3 LC-PUFAs and DHA in plasma phospholipids in multivariate analysis (Table). After correction for regression dilution bias, the relative risk associated with the highest quartile of total n-3 LC-PUFAs was 0.57 (95% CI, 0.39 – 0.82). A similar correction for DHA led to a relative risk of 0.65 (95% CI, 0.45 - 0.93). In additional multivariate analysis, adjustment for plasma phospholipid total n-3 LC-PUFAs attenuated the previous association between fish consumption and atrial fibrillation by 82% for those consuming 1 to 4 fish servings a week. These results support data from the Finnish study noted above.
In the second study, researchers led by Noelle Gronroos evaluated data from the Atherosclerosis Risk in Communities Study to determine whether the consumption of fish or plasma phospholipid levels of DHA and EPA were related to the risk of incident atrial fibrillation. There were 14,222 participants recruited from 4 US communities who averaged 54 years of age. Fish consumption was estimated from food frequency questionnaires. The investigators analyzed plasma phospholipid fatty acid concentrations in samples from 3,757 Minnesota participants. Those who had prevalent atrial fibrillation or whose race was neither white nor black or had implausible energy intakes were excluded from the analysis. The average follow-up time was 17.6 years.
The consumption of all fish, canned tuna, oily fish or other fish and of DHA plus EPA was not associated with risk of incident atrial fibrillation in multivariate analysis, regardless of the amount or type of fish consumed. Furthermore, plasma phospholipid DHA + EPA were not associated with risk for incident atrial fibrillation. For DHA alone, the association was U-shaped among the quartiles of DHA, with the greatest risk observed in the first and fourth quartiles. EPA was not associated with risk. Thus, this large cohort study supports four other prospective studies that failed to show an association between n-3 LC-PUFAs and incident atrial fibrillation. It is noteworthy that the highest quartile of tuna or baked fish consumption in the Wu study reflected more than double the amount consumed in the Gronroos
et al. study, suggesting that the amount of n-3 LC-PUFAs consumed could be important. Dose might also explain the differences observed in this study and those reported in the Finnish and Cardiovascular Health Studies for plasma phospholipid DHA concentrations.
Two additional reports bear on the relationship between n-3 LC-PUFAs or other fatty acids and incident atrial fibrillation. The first is an additional analysis from the Cardiovascular Health Study by Khawaja and colleagues who examined the relationship between total plasma free fatty acids and the risk of incident atrial fibrillation in 75-year-old US adults. The rationale for examining the association between free fatty acids and atrial fibrillation is that free fatty acids are elevated in individuals with type 2 diabetes, hypertension, obesity and inflammation who also face a higher risk of the condition. There is no previous report describing a relationship between plasma free fatty acids and atrial fibrillation risk. The sample included 4,175 participants without prevalent atrial fibrillation who had baseline fatty acid data. Atrial fibrillation risk was examined against quartiles of free fatty acids and in regression models using free fatty acids as a continuous variable, adjusting for age, gender, race and other confounding variables. After an average of 10 years’ follow-up, there was a statistically significant 29% greater risk of atrial fibrillation between the highest and lowest quartiles of free fatty acid concentrations. Analysis of the data after 5 years of follow-up, estimated the risk as 39% higher. Participants in the highest quartile of free fatty acids were older, more likely to be women and had higher adiposity, triglycerides, C-reactive protein, hypertension, type 2 diabetes and other cardiovascular risk factors. Thus, the positive association between high free fatty acid levels and risk of incident atrial fibrillation is consistent with
other reports linking higher plasma free fatty acids with different cardiac arrhythmias. Individual free fatty acids were not reported. The fourth paper in this discussion examined the differences in n-3 and n-6 PUFA content in the serum of 110 patients with atrial fibrillation, of whom 36 also had a history of ischemic heart disease. The mean age of the participants was 66 years. Two control groups were included, 46 individuals with ischemic heart disease and no atrial fibrillation and 36 healthy volunteers without atrial fibrillation or cardiac disease. Participants with atrial fibrillation in each group were further stratified by whether they had
paroxysmal or
persistent types. Participants with ischemic heart disease were more likely to have hypertension, dyslipidemia and diabetes. Those with ischemic heart disease and atrial fibrillation also had significantly larger left atria compared with healthy controls.
Patients who experienced atrial fibrillation, but did not have ischemic heart disease, had significantly higher plasma phospholipid EPA and DHA concentrations than all other groups. Although EPA concentrations were higher in the patients with both heart disease and atrial fibrillation compared with those having only ischemic heart disease, DHA concentrations did not differ among heart disease groups or controls. Patients with persistent or permanent atrial fibrillation also had higher EPA concentrations compared with controls or patients with paroxysmal atrial fibrillation. DHA concentrations were higher than controls only in patients with paroxysmal atrial fibrillation. In multivariate analysis of the risk of atrial fibrillation according to patient clinical characteristics, only EPA was statistically significant, but the risk was just 2% greater. The small numbers of patients in the groups most likely limited the strength of this analysis. The four recent papers investigating the relationship of n-3 LC-PUFAs to incident atrial fibrillation have not resolved the inconsistencies among observational studies on this topic. However, they have raised the possibility that factors such as dose of n-3 LC-PUFAs consumed, plasma free fatty acids and high plasma EPA, all might be relevant. These findings need confirmation before they can be made into nutrition recommendations. Finally, two recent meta-analyses of n-3 LC-PUFAs and atrial fibrillation suggest that cohort and randomized trials
do not support a major effect of fish or n-3 LC-PUFA consumption on reducing risk. However, n-3 LC-PUFAs
reduce risk of postoperative atrial fibrillation, but not recurrence of the condition. Wu JH, Lemaitre RN, King IB, Song X, Sacks FM, Rimm EB, Heckbert SR, Siscovick DS, Mozaffarian D. Association of plasma phospholipid long-chain omega-3 fatty acids with incident atrial fibrillation in older adults: The Cardiovascular Health Study.
Circulation 2012;125:1084-1093. [
PubMed] Gronroos NN, Chamberlain AM, Folsom AR, Soliman EZ, Agarwal SK, Nettleton JA, Alonso A. Fish, fish-derived n-3 fatty acids, and risk of incident atrial fibrillation in the Atherosclerosis Risk in Communities (ARIC) study.
PLoS One 2012;7:e36686. [
PubMed] Khawaja O, Bartz TM, Ix JH, Heckbert SR, Kizer JR, Zieman SJ, Mukamal KJ, Tracy RP, Siscovick DS, Djoussé L. Plasma free fatty acids and risk of atrial fibrillation (from the Cardiovascular Health Study).
Am J Cardiol 2012;110:212-216. [
PubMed] Tomita T, Hata T, Takeuchi T, Oguchi Y, Okada A, Aizawa K, Koshikawa M, Otagiri K, Motoki H, Kasai H, Izawa A, Koyama J, Hongo M, Ikeda U. High concentrations of omega-3 fatty acids are associated with the development of atrial fibrillation in the Japanese population.
Heart Vessels 2012; Jun 14. [Epub ahead of print] [
PubMed]
Worth noting He Z, Yang L, Tian J, Yang K, Wu J, Yao Y. Efficacy and safety of omega-3 fatty acids for the prevention of atrial fibrillation: A meta-analysis.
Can J Cardiol 2012; June 6. [Epub ahead of print] [
PubMed] Khawaja O, Gaziano JM, Djoussé L. A meta-analysis of omega-3 fatty acids and incidence of atrial fibrillation.
J Am Coll Nutr 2012;31:4-13. [
PubMed]
 Data on the relationship between long-chain omega-3 PUFAs (n-3 LC-PUFAs) and the risk of developing atrial fibrillation are notoriously inconsistent. Whether examining the risk of incident atrial fibrillation in individuals with no history of the condition, risk following coronary surgery or the odds of recurrent atrial fibrillation, reports vary from reduced risk to no association or, in a rare instance, an adverse association. Finding ways to lower the risk of atrial fibrillation is important because the condition is associated with an increased risk of stroke, myocardial infarction ventricular arrhythmia and mortality (Figure). Current risk reduction strategies focus on restoring normal sinus rhythm, controlling symptoms and preventing strokes. There would be considerable patient benefit if one could reduce the risk of developing the condition or reduce or prevent subsequent episodes.
Data on the relationship between long-chain omega-3 PUFAs (n-3 LC-PUFAs) and the risk of developing atrial fibrillation are notoriously inconsistent. Whether examining the risk of incident atrial fibrillation in individuals with no history of the condition, risk following coronary surgery or the odds of recurrent atrial fibrillation, reports vary from reduced risk to no association or, in a rare instance, an adverse association. Finding ways to lower the risk of atrial fibrillation is important because the condition is associated with an increased risk of stroke, myocardial infarction ventricular arrhythmia and mortality (Figure). Current risk reduction strategies focus on restoring normal sinus rhythm, controlling symptoms and preventing strokes. There would be considerable patient benefit if one could reduce the risk of developing the condition or reduce or prevent subsequent episodes.  Mixed findings have been reported for the consumption or status of n-3 LC-PUFAs and the risk of incident atrial fibrillation. In a recent study among older US adults without atrial fibrillation, those with higher total n-3 LC-PUFA or DHA levels in blood had a significant 29% lower risk of the condition compared with those having lower levels. Similar results were reported in a Finnish study among men. Another study of older US adults observed that those who consumed tuna or other broiled or baked fish 1 to 4 times/week had a significant 28% lower risk of incident atrial fibrillation. A study among patients hospitalized for myocardial infarction reported a significant reduction in 1-year atrial fibrillation in patients with n-3 LC-PUFA supplementation. In contrast, the Rotterdam Study of 67-year-old adults without atrial fibrillation observed no association between fish or EPA and DHA consumption with subsequent risk of the condition. Similarly, data from the Women’s Health Initiative indicated no association between fish or n-3 intakes and risk of the condition among older women. A large cohort study among Danes found no association between fish consumption and incident atrial fibrillation. In the Framingham Study, fish consumption was not associated with risk, except in a small number of participants (5 of 21 at risk) who ate more than 4 servings of dark fish per week. These individuals experienced a significantly higher risk of the condition. Two meta-analyses of randomized controlled trials on the prevention of atrial fibrillation with n-3 LC-PUFAs concluded that these fatty acids were not associated with a reduced risk of developing the condition. Two new studies have reported findings about the consumption of fish or blood levels of n-3 LC-PUFAs and the risk of incident atrial fibrillation in older adults. Jason Wu and colleagues analyzed plasma phospholipid fatty acid data from 3,326 men and women, 74 years of age on average, who were free of atrial fibrillation or heart failure at baseline. Participants were enrolled in the Cardiovascular Health Study, a community-based sample of older adults. The investigators had previously reported a significant reduction in incident atrial fibrillation among those participants who consumed tuna or other baked fish 1 to 4 times/week. However, analysis of biomarkers avoids the errors associated with dietary intake data.
Mixed findings have been reported for the consumption or status of n-3 LC-PUFAs and the risk of incident atrial fibrillation. In a recent study among older US adults without atrial fibrillation, those with higher total n-3 LC-PUFA or DHA levels in blood had a significant 29% lower risk of the condition compared with those having lower levels. Similar results were reported in a Finnish study among men. Another study of older US adults observed that those who consumed tuna or other broiled or baked fish 1 to 4 times/week had a significant 28% lower risk of incident atrial fibrillation. A study among patients hospitalized for myocardial infarction reported a significant reduction in 1-year atrial fibrillation in patients with n-3 LC-PUFA supplementation. In contrast, the Rotterdam Study of 67-year-old adults without atrial fibrillation observed no association between fish or EPA and DHA consumption with subsequent risk of the condition. Similarly, data from the Women’s Health Initiative indicated no association between fish or n-3 intakes and risk of the condition among older women. A large cohort study among Danes found no association between fish consumption and incident atrial fibrillation. In the Framingham Study, fish consumption was not associated with risk, except in a small number of participants (5 of 21 at risk) who ate more than 4 servings of dark fish per week. These individuals experienced a significantly higher risk of the condition. Two meta-analyses of randomized controlled trials on the prevention of atrial fibrillation with n-3 LC-PUFAs concluded that these fatty acids were not associated with a reduced risk of developing the condition. Two new studies have reported findings about the consumption of fish or blood levels of n-3 LC-PUFAs and the risk of incident atrial fibrillation in older adults. Jason Wu and colleagues analyzed plasma phospholipid fatty acid data from 3,326 men and women, 74 years of age on average, who were free of atrial fibrillation or heart failure at baseline. Participants were enrolled in the Cardiovascular Health Study, a community-based sample of older adults. The investigators had previously reported a significant reduction in incident atrial fibrillation among those participants who consumed tuna or other baked fish 1 to 4 times/week. However, analysis of biomarkers avoids the errors associated with dietary intake data.  The investigators measured plasma phospholipid fatty acids approximately 3 years after baseline. In a subset of samples, they evaluated the change in dietary exposure over time using blood samples obtained 13 years after baseline. With these data, they were able to adjust the regression data for regression dilution bias and estimate how usual n-3 LC-PUFA levels relate to atrial fibrillation. Consistent with their previous dietary associations, the investigators observed a significant reduction in the relative risk of incident atrial fibrillation with higher concentrations of total n-3 LC-PUFAs and DHA in plasma phospholipids in multivariate analysis (Table). After correction for regression dilution bias, the relative risk associated with the highest quartile of total n-3 LC-PUFAs was 0.57 (95% CI, 0.39 – 0.82). A similar correction for DHA led to a relative risk of 0.65 (95% CI, 0.45 - 0.93). In additional multivariate analysis, adjustment for plasma phospholipid total n-3 LC-PUFAs attenuated the previous association between fish consumption and atrial fibrillation by 82% for those consuming 1 to 4 fish servings a week. These results support data from the Finnish study noted above.
The investigators measured plasma phospholipid fatty acids approximately 3 years after baseline. In a subset of samples, they evaluated the change in dietary exposure over time using blood samples obtained 13 years after baseline. With these data, they were able to adjust the regression data for regression dilution bias and estimate how usual n-3 LC-PUFA levels relate to atrial fibrillation. Consistent with their previous dietary associations, the investigators observed a significant reduction in the relative risk of incident atrial fibrillation with higher concentrations of total n-3 LC-PUFAs and DHA in plasma phospholipids in multivariate analysis (Table). After correction for regression dilution bias, the relative risk associated with the highest quartile of total n-3 LC-PUFAs was 0.57 (95% CI, 0.39 – 0.82). A similar correction for DHA led to a relative risk of 0.65 (95% CI, 0.45 - 0.93). In additional multivariate analysis, adjustment for plasma phospholipid total n-3 LC-PUFAs attenuated the previous association between fish consumption and atrial fibrillation by 82% for those consuming 1 to 4 fish servings a week. These results support data from the Finnish study noted above. 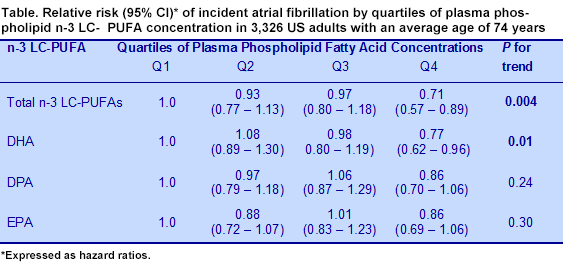 In the second study, researchers led by Noelle Gronroos evaluated data from the Atherosclerosis Risk in Communities Study to determine whether the consumption of fish or plasma phospholipid levels of DHA and EPA were related to the risk of incident atrial fibrillation. There were 14,222 participants recruited from 4 US communities who averaged 54 years of age. Fish consumption was estimated from food frequency questionnaires. The investigators analyzed plasma phospholipid fatty acid concentrations in samples from 3,757 Minnesota participants. Those who had prevalent atrial fibrillation or whose race was neither white nor black or had implausible energy intakes were excluded from the analysis. The average follow-up time was 17.6 years.
In the second study, researchers led by Noelle Gronroos evaluated data from the Atherosclerosis Risk in Communities Study to determine whether the consumption of fish or plasma phospholipid levels of DHA and EPA were related to the risk of incident atrial fibrillation. There were 14,222 participants recruited from 4 US communities who averaged 54 years of age. Fish consumption was estimated from food frequency questionnaires. The investigators analyzed plasma phospholipid fatty acid concentrations in samples from 3,757 Minnesota participants. Those who had prevalent atrial fibrillation or whose race was neither white nor black or had implausible energy intakes were excluded from the analysis. The average follow-up time was 17.6 years.  The consumption of all fish, canned tuna, oily fish or other fish and of DHA plus EPA was not associated with risk of incident atrial fibrillation in multivariate analysis, regardless of the amount or type of fish consumed. Furthermore, plasma phospholipid DHA + EPA were not associated with risk for incident atrial fibrillation. For DHA alone, the association was U-shaped among the quartiles of DHA, with the greatest risk observed in the first and fourth quartiles. EPA was not associated with risk. Thus, this large cohort study supports four other prospective studies that failed to show an association between n-3 LC-PUFAs and incident atrial fibrillation. It is noteworthy that the highest quartile of tuna or baked fish consumption in the Wu study reflected more than double the amount consumed in the Gronroos et al. study, suggesting that the amount of n-3 LC-PUFAs consumed could be important. Dose might also explain the differences observed in this study and those reported in the Finnish and Cardiovascular Health Studies for plasma phospholipid DHA concentrations.
The consumption of all fish, canned tuna, oily fish or other fish and of DHA plus EPA was not associated with risk of incident atrial fibrillation in multivariate analysis, regardless of the amount or type of fish consumed. Furthermore, plasma phospholipid DHA + EPA were not associated with risk for incident atrial fibrillation. For DHA alone, the association was U-shaped among the quartiles of DHA, with the greatest risk observed in the first and fourth quartiles. EPA was not associated with risk. Thus, this large cohort study supports four other prospective studies that failed to show an association between n-3 LC-PUFAs and incident atrial fibrillation. It is noteworthy that the highest quartile of tuna or baked fish consumption in the Wu study reflected more than double the amount consumed in the Gronroos et al. study, suggesting that the amount of n-3 LC-PUFAs consumed could be important. Dose might also explain the differences observed in this study and those reported in the Finnish and Cardiovascular Health Studies for plasma phospholipid DHA concentrations.  Two additional reports bear on the relationship between n-3 LC-PUFAs or other fatty acids and incident atrial fibrillation. The first is an additional analysis from the Cardiovascular Health Study by Khawaja and colleagues who examined the relationship between total plasma free fatty acids and the risk of incident atrial fibrillation in 75-year-old US adults. The rationale for examining the association between free fatty acids and atrial fibrillation is that free fatty acids are elevated in individuals with type 2 diabetes, hypertension, obesity and inflammation who also face a higher risk of the condition. There is no previous report describing a relationship between plasma free fatty acids and atrial fibrillation risk. The sample included 4,175 participants without prevalent atrial fibrillation who had baseline fatty acid data. Atrial fibrillation risk was examined against quartiles of free fatty acids and in regression models using free fatty acids as a continuous variable, adjusting for age, gender, race and other confounding variables. After an average of 10 years’ follow-up, there was a statistically significant 29% greater risk of atrial fibrillation between the highest and lowest quartiles of free fatty acid concentrations. Analysis of the data after 5 years of follow-up, estimated the risk as 39% higher. Participants in the highest quartile of free fatty acids were older, more likely to be women and had higher adiposity, triglycerides, C-reactive protein, hypertension, type 2 diabetes and other cardiovascular risk factors. Thus, the positive association between high free fatty acid levels and risk of incident atrial fibrillation is consistent with other reports linking higher plasma free fatty acids with different cardiac arrhythmias. Individual free fatty acids were not reported. The fourth paper in this discussion examined the differences in n-3 and n-6 PUFA content in the serum of 110 patients with atrial fibrillation, of whom 36 also had a history of ischemic heart disease. The mean age of the participants was 66 years. Two control groups were included, 46 individuals with ischemic heart disease and no atrial fibrillation and 36 healthy volunteers without atrial fibrillation or cardiac disease. Participants with atrial fibrillation in each group were further stratified by whether they had paroxysmal or persistent types. Participants with ischemic heart disease were more likely to have hypertension, dyslipidemia and diabetes. Those with ischemic heart disease and atrial fibrillation also had significantly larger left atria compared with healthy controls.
Two additional reports bear on the relationship between n-3 LC-PUFAs or other fatty acids and incident atrial fibrillation. The first is an additional analysis from the Cardiovascular Health Study by Khawaja and colleagues who examined the relationship between total plasma free fatty acids and the risk of incident atrial fibrillation in 75-year-old US adults. The rationale for examining the association between free fatty acids and atrial fibrillation is that free fatty acids are elevated in individuals with type 2 diabetes, hypertension, obesity and inflammation who also face a higher risk of the condition. There is no previous report describing a relationship between plasma free fatty acids and atrial fibrillation risk. The sample included 4,175 participants without prevalent atrial fibrillation who had baseline fatty acid data. Atrial fibrillation risk was examined against quartiles of free fatty acids and in regression models using free fatty acids as a continuous variable, adjusting for age, gender, race and other confounding variables. After an average of 10 years’ follow-up, there was a statistically significant 29% greater risk of atrial fibrillation between the highest and lowest quartiles of free fatty acid concentrations. Analysis of the data after 5 years of follow-up, estimated the risk as 39% higher. Participants in the highest quartile of free fatty acids were older, more likely to be women and had higher adiposity, triglycerides, C-reactive protein, hypertension, type 2 diabetes and other cardiovascular risk factors. Thus, the positive association between high free fatty acid levels and risk of incident atrial fibrillation is consistent with other reports linking higher plasma free fatty acids with different cardiac arrhythmias. Individual free fatty acids were not reported. The fourth paper in this discussion examined the differences in n-3 and n-6 PUFA content in the serum of 110 patients with atrial fibrillation, of whom 36 also had a history of ischemic heart disease. The mean age of the participants was 66 years. Two control groups were included, 46 individuals with ischemic heart disease and no atrial fibrillation and 36 healthy volunteers without atrial fibrillation or cardiac disease. Participants with atrial fibrillation in each group were further stratified by whether they had paroxysmal or persistent types. Participants with ischemic heart disease were more likely to have hypertension, dyslipidemia and diabetes. Those with ischemic heart disease and atrial fibrillation also had significantly larger left atria compared with healthy controls.  Patients who experienced atrial fibrillation, but did not have ischemic heart disease, had significantly higher plasma phospholipid EPA and DHA concentrations than all other groups. Although EPA concentrations were higher in the patients with both heart disease and atrial fibrillation compared with those having only ischemic heart disease, DHA concentrations did not differ among heart disease groups or controls. Patients with persistent or permanent atrial fibrillation also had higher EPA concentrations compared with controls or patients with paroxysmal atrial fibrillation. DHA concentrations were higher than controls only in patients with paroxysmal atrial fibrillation. In multivariate analysis of the risk of atrial fibrillation according to patient clinical characteristics, only EPA was statistically significant, but the risk was just 2% greater. The small numbers of patients in the groups most likely limited the strength of this analysis. The four recent papers investigating the relationship of n-3 LC-PUFAs to incident atrial fibrillation have not resolved the inconsistencies among observational studies on this topic. However, they have raised the possibility that factors such as dose of n-3 LC-PUFAs consumed, plasma free fatty acids and high plasma EPA, all might be relevant. These findings need confirmation before they can be made into nutrition recommendations. Finally, two recent meta-analyses of n-3 LC-PUFAs and atrial fibrillation suggest that cohort and randomized trials do not support a major effect of fish or n-3 LC-PUFA consumption on reducing risk. However, n-3 LC-PUFAs reduce risk of postoperative atrial fibrillation, but not recurrence of the condition. Wu JH, Lemaitre RN, King IB, Song X, Sacks FM, Rimm EB, Heckbert SR, Siscovick DS, Mozaffarian D. Association of plasma phospholipid long-chain omega-3 fatty acids with incident atrial fibrillation in older adults: The Cardiovascular Health Study. Circulation 2012;125:1084-1093. [PubMed] Gronroos NN, Chamberlain AM, Folsom AR, Soliman EZ, Agarwal SK, Nettleton JA, Alonso A. Fish, fish-derived n-3 fatty acids, and risk of incident atrial fibrillation in the Atherosclerosis Risk in Communities (ARIC) study. PLoS One 2012;7:e36686. [PubMed] Khawaja O, Bartz TM, Ix JH, Heckbert SR, Kizer JR, Zieman SJ, Mukamal KJ, Tracy RP, Siscovick DS, Djoussé L. Plasma free fatty acids and risk of atrial fibrillation (from the Cardiovascular Health Study). Am J Cardiol 2012;110:212-216. [PubMed] Tomita T, Hata T, Takeuchi T, Oguchi Y, Okada A, Aizawa K, Koshikawa M, Otagiri K, Motoki H, Kasai H, Izawa A, Koyama J, Hongo M, Ikeda U. High concentrations of omega-3 fatty acids are associated with the development of atrial fibrillation in the Japanese population. Heart Vessels 2012; Jun 14. [Epub ahead of print] [PubMed] Worth noting He Z, Yang L, Tian J, Yang K, Wu J, Yao Y. Efficacy and safety of omega-3 fatty acids for the prevention of atrial fibrillation: A meta-analysis. Can J Cardiol 2012; June 6. [Epub ahead of print] [PubMed] Khawaja O, Gaziano JM, Djoussé L. A meta-analysis of omega-3 fatty acids and incidence of atrial fibrillation. J Am Coll Nutr 2012;31:4-13. [PubMed]
Patients who experienced atrial fibrillation, but did not have ischemic heart disease, had significantly higher plasma phospholipid EPA and DHA concentrations than all other groups. Although EPA concentrations were higher in the patients with both heart disease and atrial fibrillation compared with those having only ischemic heart disease, DHA concentrations did not differ among heart disease groups or controls. Patients with persistent or permanent atrial fibrillation also had higher EPA concentrations compared with controls or patients with paroxysmal atrial fibrillation. DHA concentrations were higher than controls only in patients with paroxysmal atrial fibrillation. In multivariate analysis of the risk of atrial fibrillation according to patient clinical characteristics, only EPA was statistically significant, but the risk was just 2% greater. The small numbers of patients in the groups most likely limited the strength of this analysis. The four recent papers investigating the relationship of n-3 LC-PUFAs to incident atrial fibrillation have not resolved the inconsistencies among observational studies on this topic. However, they have raised the possibility that factors such as dose of n-3 LC-PUFAs consumed, plasma free fatty acids and high plasma EPA, all might be relevant. These findings need confirmation before they can be made into nutrition recommendations. Finally, two recent meta-analyses of n-3 LC-PUFAs and atrial fibrillation suggest that cohort and randomized trials do not support a major effect of fish or n-3 LC-PUFA consumption on reducing risk. However, n-3 LC-PUFAs reduce risk of postoperative atrial fibrillation, but not recurrence of the condition. Wu JH, Lemaitre RN, King IB, Song X, Sacks FM, Rimm EB, Heckbert SR, Siscovick DS, Mozaffarian D. Association of plasma phospholipid long-chain omega-3 fatty acids with incident atrial fibrillation in older adults: The Cardiovascular Health Study. Circulation 2012;125:1084-1093. [PubMed] Gronroos NN, Chamberlain AM, Folsom AR, Soliman EZ, Agarwal SK, Nettleton JA, Alonso A. Fish, fish-derived n-3 fatty acids, and risk of incident atrial fibrillation in the Atherosclerosis Risk in Communities (ARIC) study. PLoS One 2012;7:e36686. [PubMed] Khawaja O, Bartz TM, Ix JH, Heckbert SR, Kizer JR, Zieman SJ, Mukamal KJ, Tracy RP, Siscovick DS, Djoussé L. Plasma free fatty acids and risk of atrial fibrillation (from the Cardiovascular Health Study). Am J Cardiol 2012;110:212-216. [PubMed] Tomita T, Hata T, Takeuchi T, Oguchi Y, Okada A, Aizawa K, Koshikawa M, Otagiri K, Motoki H, Kasai H, Izawa A, Koyama J, Hongo M, Ikeda U. High concentrations of omega-3 fatty acids are associated with the development of atrial fibrillation in the Japanese population. Heart Vessels 2012; Jun 14. [Epub ahead of print] [PubMed] Worth noting He Z, Yang L, Tian J, Yang K, Wu J, Yao Y. Efficacy and safety of omega-3 fatty acids for the prevention of atrial fibrillation: A meta-analysis. Can J Cardiol 2012; June 6. [Epub ahead of print] [PubMed] Khawaja O, Gaziano JM, Djoussé L. A meta-analysis of omega-3 fatty acids and incidence of atrial fibrillation. J Am Coll Nutr 2012;31:4-13. [PubMed]

